
General information
Due to the development of intervertebral disc chondrosis, the human body has lost its shock absorption properties, inherent mobility and elasticity. Usually, this spinal disease is very common, and the severity of most people varies from one or more to 40 years old. According to the affected part of the spine in clinical practice, it is possible to distinguish cervical, lumbar and sternal osteochondrosis, and their mixed forms, which are considered the most difficult.
The thoracic osteochondrosis discussed in this article is the rarest form of this pathology, especially due to the anatomical structure of the upper part of the human bone. Therefore, in the chest area, the osteochondral system is composed of 12 vertebrae, which are connected by joints with ribs, and the front ends of the ribs are connected to the relatively whole sternum. This bone structure provides a strong and strong frame to protect the thoracic organs (heart, lungs) from injury. In addition, the vertebrae of this part of the spine are characterized by the small height and long length of the spinous processes, which gives them a view of the closely arranged tiles. All these together limit the mobility of this part of the back and the negative effects of physical activity on it, thereby protecting the intervertebral disc from damage.
As another reason for the lower frequency of detecting thoracic osteochondrosis, compared with lumbar and cervical osteochondrosis, there is a physiological kyphosis in this area (the spine is naturally bent backward), so most of the external load fallsOn the anterior and lateral fragments of the vertebrae and intervertebral discs. As the pathological process of the motor segments of the spine develops, these areas are mainly exposed to degeneration. However, since they have no changes in nerve endings and spinal cord membranes, pain is usually not observed. However, in some cases, the negative transformation of the thoracic spine can affect the posterior fractures of the intervertebral disc and vertebrae and/or vertebral-costal joints, usually resulting in compression of the spinal nerve roots. In this case, thoracic osteochondrosis is accompanied by radiation syndrome, which has been accompanied by various local pains (sometimes very remote), and has violated the functions of many human organs (liver, lung, pancreas, heart, etc. ).
Because of the ambiguous and diverse manifestations of sternochondrosis, doctors often refer to this pathological form as "chameleon disease" because it can be cleverly disguised as symptoms of respiratory and digestive tract diseases, heart muscles, etc. In this case, the correct differential diagnosis is very important. Various specific studies will help determine the symptoms and treatment of thoracic osteochondrosis.
The strategy and effectiveness of further treatment will largely depend on the progress of the degenerative dystrophy process in the spinal tissue. This pathology has been recognized at the early stage of disease development, and it is of great significance to improve the patient’s condition. It is entirely possible to exercise with simple physical therapy techniques and exercise therapy, but if it is discovered later, it may require complicated surgery. surgery. This is why vertebral orthopedists strongly recommend that you seek expert help as soon as possible for any early and/or long-term back pain.
Pathogenesis
The incidence of thoracic osteochondrosis in men and women is actually the same, because in the pathogenesis of this disease, there is no gender tendency to cause intervertebral disc degeneration. However, years of clinical experience in the treatment of osteochondrosis have shown that the earliest symptoms of men are earlier than the age of similar negative symptoms in women. In particular, this is due to the fact that estrogen can protect women’s tissues up to a certain age, and estrogen can reduce its levels.
According to statistical evidence, vertebral osteochondrosis of varying severity is usually found in most elderly people, which automatically classifies it as an age-related disease. At the same time, after the last time, this pathology will significantly "rejuvenate" until it has appeared before school age. Therefore, the exact etiology and initial pathogenesis of osteochondrosis of the spine have not yet been determined. At one time, more than ten theories about its origin and development were developed, including hormones, infectiousness, mechanical, vascular, hereditary, allergic, etc. , but in practice, none of them have been fully confirmed.
Today, doctors explain the occurrence of osteochondrosis by the sum of the complementary negative effects on the spinal tissue. Among them, they emphasize that one or more spinal movements are continuously overloaded by two adjacent vertebrae (upper andLower part) and the segment formed by the intervertebral disc in the middle. Paradoxically, this overload may be the result of excessive physical work on the spine and its long-term unnatural back position. For example, long hours of work or sitting at a table and studying is one of the main factors in the development of vertebral structure degenerative dystrophy.
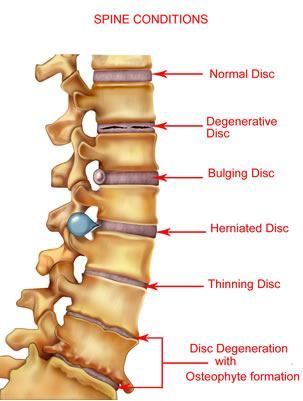
The initial formation or aggravation of thoracic osteochondrosis may be affected by malnutrition, uneven development of the back and pectoral muscles, overweight (obesity), pathology of the lower limbs (for example, flat feet), back injuries, etc. In the pathogenesis of this disease, the disturbance of the segmental blood circulation plays an important role, which can lead to the dehydration of the dental pulp (colloid) nucleus, which in turn leads to a decrease in the amortized quality of the intervertebral disc, changes in the load on the surrounding fibrous annulus, andThe further progressive destruction of the spine motion segment.
During its development, sternal osteochondrosis has gone through four consecutive stages of development. Each stage is characterized by intervertebral discs. The structures of adjacent vertebrae and facets have their own anatomical and morphological changes in joints. In addition, the negative metamorphosis that accompanies this disease can directly affect other nearby tissues (muscles, blood vessels, connective tissue), or indirectly affect the work of distant organs and systems in the body. (Intestines, heart, lungs, etc. ).
Level 1
In the initial stage of the formation of sternal osteochondrosis, microcracks are formed in the inner membrane of the annulus fibrosus, and the nucleus pulposus gradually begins to penetrate into it, thereby stimulating the nerve ending annulus and the posterior longitudinal ligament at the end of the fiber. At this stage of the disease, the patient may already feel soreness directly in the middle of the back or pain in the heart area. He will also be troubled by convulsions. In the back muscles.
Second degree
2nd degree thoracic chondrochondrosis is characterized by further destruction of the annulus fibrosus and spinal instability, which is caused by excessive movement of the affected vertebrae. The second stage of the painful pathological development feels intensified, and may continue to develop with back pain (mild persistent pain, aggravated back movement) or back pain (a sharp increase in the background of staying in one position for a long time). The pain of shooting).
Three Degrees
Fourth Degree
Reason
Sternal osteochondrosis in men and women can develop due to the following predisposing factors:
- Genetic predisposition leads to abnormal formation of spinal motion segments;
- A lifestyle that lacks physical activity, leading to back muscle dystrophy;
- Strength exercise, including excessive mechanical stress on the spine (mainly lifting weights);
- Spinal injuries (even injuries that occurred in the distant past); The endocrine disorder of the human body destroys the nutrition of the spine tissue;
- Significantly higher than normal weight (obesity);
- Unhealthy diet (deficiencies in vitamins, minerals and fluids);
- Pathology of the spine, unnatural curvature;
- Unbalanced muscle frame development;
- Study for a long time or work in a sitting position with the body bent forward;
- Physically difficult working conditions (continuous improper weight lifting);
- Severe metabolic disorder;
- Flat feet and other diseases of lower limbs affect the redistribution of spine load;
- Vascular diseases that damage the blood supply to the back;
- Serious infections, allergies and autoimmune processes;
- Hypothermia;
- Nervous situation and nervous exhaustion;
- Bad habits and smoking.
Symptoms of thoracic osteochondrosis
Due to the above structural characteristics of this part of the spine, the signs of sternal osteochondrosis may not directly trouble the patient for a long time, and only appear when the pathological process spreads to the outside and/or after the affected spinal motion segmentDepartment and disease transition to the second or third degree. Generally speaking, all symptoms of sternal osteochondrosis are manifested in the form of vertebral syndrome (the effect of pain is directly related to the functional disease of the bone-cartilage tissue of the spine) and extravertebral or compression syndrome (pathology of the spineNegative phenomenon caused by sexual drive).
Vertebral Syndrome
The vertebral symptoms of spine thoracic chondrosis are mainly manifested in two pain syndromes, called back pain and back pain.
Dorsago
This is an acute and sudden onset of pain, the so-called "lower back pain", which is located in the shoulder interspace and can occur at any time. In most cases, dorsago syndrome affects the sitting posture, where the body leans forward and changes the position of the body drastically. The patient described the moment of the attack as a "dagger blow, " accompanied by severe spinal muscle spasms. In addition to severe pain, the subjective sensation of the back is manifested as shortness of breath, and it severely limits the freedom of movement of the back and chest. Periodic episodes of similar deterioration of osteochondrosis may last up to two weeks.
Backache
The difference between this syndrome and previous syndromes is that the gradual discomfort and pain may increase in two to three weeks. The pain itself of backache is not obvious, but long-term existence can lead to persistent anxiety. The back muscles and back muscles are under a lot of pressure, which may make the patient feel that the intake of air is insufficient. Backache increases with trunk movement (especially when bending over), deep breathing, coughing, etc. They are upper back pain (the main location of the negative phenomenon in the spine, neck and thoracic segment) and lower back pain (the main negative location of the spine and neck pain) in the thoracolumbar spine.
Extravertebral syndrome
The extravertebral syndrome of sternal osteochondrosis, due to the maximum extent of this part of the spine, may be very diverse, which greatly complicates the correct diagnosis of the disease. They are mechanically compressed corresponding nerve roots, nearby blood vessels or the spinal cord itself. Compression symptoms in men and women are usually similar, and only the pathological impulse is transmitted to the sex bulb (for example, in men, erectile dysfunction sometimes occurs with this disease as the background). In almost all cases, extravertebral symptoms are caused by an already formed intervertebral hernia, which usually appears in the lower thoracic area, but in principle they can form in any spinal movement from the D1 vertebra to the D12 vertebra. As you can see in the figure below, the reason for participating in pathological diseases is the process of locating certain human systems and organs with negative characteristics of osteochondrosis.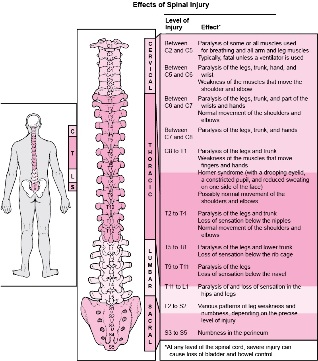
Root nerve syndrome
In the framework of the compression symptoms of sternochondrosis, nerve root syndrome is most often and clearly observed, which is caused by compression of one or another nerve ending in the spine. Depending on the concentration, for example, the following painful phenomena may trouble the patient:
- In the case of the invasion of the T1 vertebral area-the pain and paresthesia of the upper thoracic spine usually spreads along the upper cap area of the shoulder to one of the armpits to the area of the elbow joint;
- In the case of invasion of the T2-T6 vertebral area-pain such as intercostal neuralgia can extend from this part of the spine along the interstitial area of the shoulder, and surround the armpit and shoulder in a semicircle and 2-6 intercostal spacescap bone area to sternum
- If infringement occurs in the T7-T8 vertebrae region-waistband pain mainly spreads from the low position of the shoulder blade of the spine-costal joint to the upper part of the costal arch and affects the upper abdominal area, causing muscle defense (strong muscle tension);
- If the T9-T10 vertebrae area is invaded-intercostal neuralgia extends from the spinal motion segment of the lower chest to the lower part of the costal arch, and then to the umbilicus, thereby changing the tone of the middle part of the abdominal muscles;
- If the T11-T12 vertebra area is invaded-the pain also emanates from the spinal movement of the lower chest and travels along the corresponding lateral area of the chest to the lower stomach (below the stomach) and groin area.
Therefore, when the osteochondrosis process is located in the upper chest area of the spine (from T1 to T4), the patient may experience soreness and/or various discomforts in the esophagus or pharynx, which is usually considered the presence of foreign bodies. This feeling is usually paroxysmal (sometimes permanent) and adds to the burden on the problematic part of the back. Sometimes the manifestations of upper thoracic nerve root syndrome are confused with signs of obstructive bronchitis or pneumonia, because reflex cough with sternal osteochondrosis and chest pain are similar to the symptoms of this group of diseases. In addition, chest pain may appear in the form of chest pain, which is reminiscent of the intensity of angina pectoris, pulmonary thromboembolism, myocardial infarction, and other similar pathologies of serious nature, requiring a detailed analysis of the difference by the doctor.
Patients with sternal osteochondrosis in the middle spine (T5 to T7) most often suffer from discomfort and pain in the solar plexus and stomach, called vertebral stomach pain. When the spine movement segment T8-T9 fails, it is possible to produce pain in the duodenum, which is called-spine duodenal pain. . . The intensity of those and other painful feelings in different patients or in different patients varies from mild and "The pain" is extremely severe, and the time varies. Usually, in the case of sudden body movements, they will prolong the body's long stay in one position (sitting on a table, lying on your back, etc. ), and when sneezing or coughing. These pains are usually accompanied by paresthesias. (Numbness, tingling, burning) in the middle of the abdominal wall.
If radial osteochondrosis occurs in the lower thoracic region of the spine (from T8 to T12), some patients may complain of pain in the lower abdominal cavity, mimicking bowel disease or pathology. Sometimes the soreness spreads to the gallbladder and is located in the sagging cartilage area on the right side. In even lesser cases, patients experience pain similar to clinical symptoms of bladder pathology in the suprapubic area. As before, in this case, the nature of this pain can vary within a considerable range (from mild to severe), and with prolonged physical or static pressure on the spine, sneezing, coughing, etc. The severity will also increase.
Compressive myelopathy
This compression syndrome of sternal osteochondrosis is very rare. It is a compression of the spinal cord directly caused by an intervertebral hernia. . . At first, the characteristic symptoms are formed by the back or waistband pain in the problem area. Local pain, as well as weakness and/or numbness in the legs. As the disease progresses, the pain increases, which will affect the downstream intercostal space, abdominal organs, groin area and lower limbs. Severe spinal cord compression may develop pelvic organ dysfunction, leading to disrupted defecation and/or urination. In addition, there may be severe superficial and deep paresthesias and sensory disturbances, up to spastic paresthesias in one or even two legs.
Vascular compression
Compression of blood vessels adjacent to the thoracic spine causes bone marrow ischemia. As a result, blood supply is interrupted, which leads to proper nutrition of the spinal cord. The manifestation of this syndrome is actually a complete repetition of the symptoms of compressive myelopathy. The main feature is pelvic disease, loss of sensation and decreased function of the lower limbs. Patients often describe problems with the phrase "failure of both legs".
Nutrition syndrome
In many cases, the autonomic ganglion (ganglion) associated with sternal osteochondrosis is damaged, so the patient may experience various adverse symptoms. These may be various paresthesias. , Skin itching and skin pigmentation changes in the problematic ganglion area, burning pain in half of the body, local temperature disturbance, muscle hypertrophy or weight loss, limbs or internal organs working disorder, etc. According to him, the symptoms of these visceral vertebrae are similar to the manifestations of Radiation Nerve Syndrome, but they are different in the absence of clear positioning and secretion and movement disorders. When it comes to the pathological process of the stellar body, a nodule affecting the upper thoracic spine may have an invasion in the arms, upper chest and heart. If the lower thoracic ganglia are damaged, dysfunction may occur. Nutritional changes in the small pelvic organs, abdominal and thoracic cavity, as well as the lower limbs and the rest of the body.



































